Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems. Body mass index (BMI), a measurement which compares weight and height, defines people as overweight (pre-obese) if their BMI is between 25 kg/m2 and 30 kg/m2, and obese when it is greater than 30 kg/m2.
Obesity increases the likelihood of various diseases, particularly heart disease, type 2 diabetes, breathing difficulties during sleep, certain types of cancer, and osteoarthritis. Obesity is most commonly caused by a combination of excessive dietary calories, lack of physical activity, and genetic susceptibility, although a few cases are caused primarily by genes, endocrine disorders, medications or psychiatric illness. Evidence to support the view that some obese people eat little yet gain weight due to a slow metabolism is limited; on average obese people have a greater energy expenditure than their thin counterparts due to the energy required to maintain an increased body mass.
Dieting and physical exercise are the mainstays of treatment for obesity. To supplement this, or in case of failure, anti-obesity drugs may be taken to reduce appetite or inhibit fat absorption. In severe cases, surgery is performed or an intragastric balloon is placed to reduce stomach volume and/or bowel length, leading to earlier satiation and reduced ability to absorb nutrients from food.
Obesity is a leading preventable cause of death worldwide, with increasing prevalence in adults and children, and authorities view it as one of the most serious public health problems of the 21st century. Obesity is stigmatized in much of the modern world (particularly in the Western world), though it was widely perceived as a symbol of wealth and fertility at other times in history, and still is in some parts of the world.
Classification
Classification of obesity
Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health. It is defined by body mass index (BMI) and further evaluated in terms of fat distribution via the waist–hip ratio and total cardiovascular risk factors. BMI is closely related to both percentage body fat and total body fat.
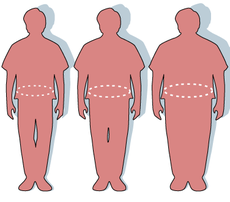
A "super obese" male with a BMI of 47 kg/m2: weight 146 kg (322 lb), height 177 cm (5 ft 10 in)
In children, a healthy weight varies with age and sex. Obesity in children and adolescents is defined not as an absolute number, but in relation to a historical normal group, such that obesity is a BMI greater than the 95th percentile. The reference data on which these percentiles are based are from 1963 to 1994, and thus have not been affected by the recent increases in weight.
BMI Classification
< 18.5 underweight 18.5–24.9 normal weight 25.0–29.9 overweight 30.0–34.9 class I obesity 35.0–39.9 class II obesity ≥ 40.0 class III obesity BMI is calculated by dividing the subject's mass by the square of his or her height, typically expressed either in metric or US "customary" units: Metric: BMI = kilograms / meters2 US customary and imperial: BMI = lb * 703 / in2 where lb is the subject's weight in pounds and in is the subject's height in inches. The most commonly used definitions, established by the World Health Organization (WHO) in 1997 and published in 2000, provide the values listed in the table at right. Some modifications to the WHO definitions have been made by particular bodies. The surgical literature breaks down "class III" obesity into further categories whose exact values are still disputed. Any BMI ≥ 35 or 40 is severe obesity A BMI of ≥ 35 or 40–44.9 or 49.9 is morbid obesity A BMI of ≥ 45 or 50 is super obese As Asian populations develop negative health consequences at a lower BMI than Caucasians, some nations have redefined obesity; the Japanese have defined obesity as any BMI greater than 25 while China uses a BMI of greater than 28. Effects on health Excessive body weight is associated with various diseases, particularly cardiovascular diseases, diabetes mellitus type 2, obstructive sleep apnea, certain types of cancer, and osteoarthritis. As a result, obesity has been found to reduce life expectancy. Mortality Relative risk of death for men (left) and women (right) in the United States by BMI. Obesity is one of the leading preventable causes of death worldwide. Large-scale American and European studies have found that mortality risk is lowest at a BMI of 22.5–25 kg/m2 in non-smokers and at 24–27 kg/m2 in current smokers, with risk increasing along with changes in either direction. A BMI above 32 has been associated with a doubled mortality rate among women over a 16-year period.[ In the United States obesity is estimated to cause an excess 111,909 to 365,000 death per year, while 1 million (7.7%) of deaths in the European Union are attributed to excess weight. On average, obesity reduces life expectancy by six to seven years: a BMI of 30–35 reduces life expectancy by two to four years, while severe obesity (BMI > 40) reduces life expectancy by 10 years.
Morbidity
Obesity-associated morbidity
Obesity increases the risk of many physical and mental conditions. These comorbidities are most commonly shown in metabolic syndrome, a combination of medical disorders which includes: diabetes mellitus type 2, high blood pressure, high blood cholesterol, and high triglyceride levels.
Complications are either directly caused by obesity or indirectly related through mechanisms sharing a common cause such as a poor diet or a sedentary lifestyle. The strength of the link between obesity and specific conditions varies. One of the strongest is the link with type 2 diabetes. Excess body fat underlies 64% of cases of diabetes in men and 77% of cases in women.
Health consequences fall into two broad categories: those attributable to the effects of increased fat mass (such as osteoarthritis, obstructive sleep apnea, social stigmatization) and those due to the increased number of fat cells (diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease). Increases in body fat alter the body's response to insulin, potentially leading to insulin resistance. Increased fat also creates a proinflammatory state, and a prothrombotic state.
Medical field Condition Medical field Condition
Cardiology
ischemic heart disease: angina and myocardial infarction
congestive heart failure
high blood pressure
abnormal cholesterol levels
deep vein thrombosis and pulmonary embolism
Dermatology
stretch marks
acanthosis nigricans
lymphedema
cellulitis
hirsutism
intertrigo
Endocrinology and Reproductive medicine
diabetes mellitus
polycystic ovarian syndrome
menstrual disorders
infertility
complications during pregnancy
birth defects
intrauterine fetal death
Gastrointestinal
gastroesophageal reflux disease
fatty liver disease
cholelithiasis (gallstones)
Neurology
stroke
meralgia paresthetica
migraines
carpal tunnel syndrome
dementia
idiopathic intracranial hypertension
multiple sclerosis
Oncology
breast, ovarian
esophageal, colorectal
liver, pancreatic
gallbladder, stomach
endometrial, cervical
prostate, kidney
non-Hodgkin's lymphoma, multiple myeloma
Psychiatry
depression in women
social stigmatization
Respirology
obstructive sleep apnea
obesity hypoventilation syndrome
asthma
increased complications during general anaesthesia
Rheumatology and Orthopedics
gout
poor mobility
osteoarthritis
low back pain
Urology and Nephrology
erectile dysfunction
urinary incontinence
chronic renal failure
hypogonadism
Obesity survival paradox
Obesity paradox
Although the negative health consequences of obesity in the general population are well supported by the available evidence, health outcomes in certain subgroups seem to be improved at an increased BMI, a phenomenon known as the obesity survival paradox. The paradox was first described in 1999 in overweight and obese people undergoing hemodialysis, and has subsequently been found in those with heart failure and peripheral artery disease (PAD).
In people with heart failure, those with a BMI between 30.0–34.9 had lower mortality than those with a normal weight. This has been attributed to the fact that people often lose weight as they become progressively more ill. Similar findings have been made in other types of heart disease. People with class I obesity and heart disease do not have greater rates of further heart problems than people of normal weight who also have heart disease. In people with greater degrees of obesity, however, risk of further events is increased. Even after cardiac bypass surgery, no increase in mortality is seen in the overweight and obese. One study found that the improved survival could be explained by the more aggressive treatment obese people receive after a cardiac event. Another found that if one takes into account chronic obstructive pulmonary disease (COPD) in those with PAD the benefit of obesity no longer exists.
Causes
At an individual level, a combination of excessive caloric intake and a lack of physical activity is thought to explain most cases of obesity.] A limited number of cases are due primarily to genetics, medical reasons, or psychiatric illness. In contrast, increasing rates of obesity at a societal level are felt to be due to an easily accessible and palatable diet, increased reliance on cars, and mechanized manufacturing.
A 2006 review identified ten other possible contributors to the recent increase of obesity: (1) insufficient sleep, (2) endocrine disruptors (environmental pollutants that interfere with lipid metabolism), (3) decreased variability in ambient temperature, (4) decreased rates of smoking, because smoking suppresses appetite, (5) increased use of medications that can cause weight gain (e.g., atypical antipsychotics), (6) proportional increases in ethnic and age groups that tend to be heavier, (7) pregnancy at a later age (which may cause susceptibility to obesity in children), (8) epigenetic risk factors passed on generationally, (9) natural selection for higher BMI, and (10) assortative mating leading to increased concentration of obesity risk factors (this would not necessarily increase the number of obese people, but would increase the average population weight). While there is substantial evidence supporting the influence of these mechanisms on the increased prevalence of obesity, the evidence is still inconclusive, and the authors state that these are probably less influential than the ones discussed in the previous paragraph.
Diet
Diet and obesity
Map of dietary energy availability per person per day in 1961 (left) and 2001–2003 (right) in kcal/person/day.
no data
<1600 1600–1800 1800–2000 2000–2200 2200–2400 2400–2600 2600–2800 2800–3000 3000–3200 3200–3400 3400–3600 >3600
Average per capita energy consumption of the world from 1961 to 2002
The per capita dietary energy supply varies markedly between different regions and countries. It has also changed significantly over time. From the early 1970s to the late 1990s the average calories available per person per day (the amount of food bought) has increased in all parts of the world except Eastern Europe. The United States had the highest availability with 3,654 calories per person in 1996. This increased further in 2003 to 3,754. During the late 1990s Europeans had 3,394 calories per person, in the developing areas of Asia there were 2,648 calories per person, and in sub-Saharan Africa people had 2,176 calories per person. Total calorie consumption has been found to be related to obesity.
The widespread availability of nutritional guidelines has done little to address the problems of overeating and poor dietary choice. From 1971 to 2000, obesity rates in the United States increased from 14.5% to 30.9%. During the same period, an increase occurred in the average amount of calories consumed. For women, the average increase was 335 calories per day (1,542 calories in 1971 and 1,877 calories in 2004), while for men the average increase was 168 calories per day (2,450 calories in 1971 and 2,618 calories in 2004). Most of these extra calories came from an increase in carbohydrate consumption rather than fat consumption. The primary sources of these extra carbohydrates are sweetened beverages, which now account for almost 25 percent of daily calories in young adults in America. Consumption of sweetened drinks is believed to be contributing to the rising rates of obesity.
As societies become increasingly reliant on energy-dense, big-portion, fast-food meals, the association between fast-food consumption and obesity becomes more concerning. In the United States consumption of fast-food meals tripled and calorie intake from these meals quadrupled between 1977 and 1995.
Agricultural policy and techniques in the United States and Europe have led to lower food prices. In the United States, subsidization of corn, soy, wheat, and rice through the U.S. farm bill has made the main sources of processed food cheap compared to fruits and vegetables.
Obese people consistently under-report their food consumption as compared to people of normal weight. This is supported both by tests of people carried out in a calorimeter room and by direct observation.
Sedentary lifestyle
Sedentary lifestyle and Exercise trends
A sedentary lifestyle plays a significant role in obesity. Worldwide there has been a large shift towards less physically demanding work, and currently at least 60% of the world's population gets insufficient exercise. This is primarily due to increasing use of mechanized transportation and a greater prevalence of labor-saving technology in the home. In children, there appear to be declines in levels of physical activity due to less walking and physical education. World trends in active leisure time physical activity are less clear. The World Health Organization indicates people worldwide are taking up less active recreational pursuits, while a study from Finland[88] found an increase and a study from the United States found leisure-time physical activity has not changed significantly.
In both children and adults, there is an association between television viewing time and the risk of obesity. A 2008 meta-analysis found 63 of 73 studies (86%) showed an increased rate of childhood obesity with increased media exposure, with rates increasing proportionally to time spent watching television.
Genetics
Genetics of obesity
A 1680 painting by Juan Carreno de Miranda of a girl presumed to have Prader-Willi syndrome
Like many other medical conditions, obesity is the result of an interplay between genetic and environmental factors. Polymorphisms in various genes controlling appetite and metabolism predispose to obesity when sufficient calories are present. As of 2006 more than 41 of these sites have been linked to the development of obesity when a favorable environment is present. People with two copies of the FTO gene (fat mass and obesity associated gene) has been found on average to weight 3-4 kg more and have a 1.67-fold greater risk of obesity compared to those without the risk allele. The percentage of obesity that can be attributed to genetics varies, depending on the population examined, from 6% to 85%.
Obesity is a major feature in several syndromes, such as Prader-Willi syndrome, Bardet-Biedl syndrome, Cohen syndrome, and MOMO syndrome. (The term "non-syndromic obesity" is sometimes used to exclude these conditions.) In people with early-onset severe obesity (defined by an onset before 10 years of age and body mass index over three standard deviations above normal), 7% harbor a single point DNA mutation.
Studies that have focused upon inheritance patterns rather than upon specific genes have found that 80% of the offspring of two obese parents were obese, in contrast to less than 10% of the offspring of two parents who were of normal weight.
The thrifty gene hypothesis postulates that certain ethnic groups may be more prone to obesity in an equivalent environment. Their ability to take advantage of rare periods of abundance by storing energy as fat would be advantageous during times of varying food availability, and individuals with greater adipose reserves would be more likely survive famine. This tendency to store fat, however, would be maladaptive in societies with stable food supplies. This is the presumed reason that Pima Indians, who evolved in a desert ecosystem, developed some of the highest rates of obesity when exposed to a Western lifestyle.
Medical and psychiatric illness
Certain physical and mental illnesses and the pharmaceutical substances used to treat them can increase risk of obesity. Medical illnesses that increase obesity risk include several rare genetic syndromes (listed above) as well as some congenital or acquired conditions: hypothyroidism, Cushing's syndrome, growth hormone deficiency, and the eating disorders: binge eating disorder and night eating syndrome However, obesity is not regarded as a psychiatric disorder, and therefore is not listed in the DSM-IVR as a psychiatric illness. The risk of overweight and obesity is higher in patients with psychiatric disorders than in persons without psychiatric disorders.
Certain medications may cause weight gain or changes in body composition; these include insulin, sulfonylureas, thiazolidinediones, atypical antipsychotics, antidepressants, steroids, certain anticonvulsants (phenytoin and valproate), pizotifen, and some forms of hormonal contraception.
Social determinants
Social determinants of obesity
While genetic influences are important to understanding obesity, they cannot explain the current dramatic increase seen within specific countries or globally. Though it is accepted that calorie consumption in excess of calorie expenditure leads to obesity on an individual basis, the cause of the shifts in these two factors on the societal scale is much debated. There are a number of theories as to the cause but most believe it is a combination of various factors.
The correlation between social class and BMI varies globally. A review in 1989 found that in developed countries women of a high social class were less likely to be obese. No significant differences were seen among men of different social classes. In the developing world, women, men, and children from high social classes had greater rates of obesity. An update of this review carried out in 2007 found the same relationships, but they were weaker. The decrease in strength of correlation was felt to be due to the effects of globalization. Among developed countries, levels of adult obesity, and percentage of teenage children who are overweight, are correlated with income inequality. A similar relationship is seen between US states: more adults, even in higher social classes, are obese in more unequal states.
Many explanations have been put forth for associations between BMI and social class. It is thought that in developed countries, the wealthy are able to afford more nutritious food, they are under greater social pressure to remain slim, and have more opportunities along with greater expectations for physical fitness. In undeveloped countries the ability to afford food, high energy expenditure with physical labor, and cultural values favoring a larger body size are believed to contribute to the observed patterns. Attitudes toward body mass held by people in one's life may also play a role in obesity. A correlation in BMI changes over time has been found between friends, siblings, and spouses. Stress and perceived low social status appear to increase risk of obesity.
Smoking has a significant effect on an individual's weight. Those who quit smoking gain an average of 4.4 kilograms (9.7 lb) for men and 5.0 kilograms (11.0 lb) for women over ten years. However, changing rates of smoking have had little effect on the overall rates of obesity.
In the United States the number of children a person has is related to their risk of obesity. A woman's risk increases by 7% per child, while a man's risk increases by 4% per child. This could be partly explained by the fact that having dependent children decreases physical activity in Western parents.
In the developing world urbanization is playing a role in increasing rate of obesity. In China overall rates of obesity are below 5%; however, in some cities rates of obesity are greater than 20%.
Malnutrition in early life is believed to play a role in the rising rates of obesity in the developing world. Endocrine changes that occur during periods of malnutrition may promote the storage of fat once more calories become available.
Infectious agents
See also: Infectobesity
The study of the effect of infectious agents on metabolism is still in its early stages. Gut flora has been shown to differ between lean and obese humans. There is an indication that gut flora in obese and lean individuals can affect the metabolic potential. This apparent alteration of the metabolic potential is believed to confer a greater capacity to harvest energy contributing to obesity. Whether these differences are the direct cause or the result of obesity has yet to be determined unequivocally.
An association between viruses and obesity has been found in humans and several different animal species. The amount that these associations may have contributed to the rising rate of obesity is yet to be determined.
Pathophysiology
Flier summarizes the many possible pathophysiological mechanisms involved in the development and maintenance of obesity. This field of research had been almost unapproached until leptin was discovered in 1994. Since this discovery, many other hormonal mechanisms have been elucidated that participate in the regulation of appetite and food intake, storage patterns of adipose tissue, and development of insulin resistance. Since leptin's discovery, ghrelin, insulin, orexin, PYY 3-36, cholecystokinin, adiponectin, as well as many other mediators have been studied. The adipokines are mediators produced by adipose tissue; their action is thought to modify many obesity-related diseases.
Leptin and ghrelin are considered to be complementary in their influence on appetite, with ghrelin produced by the stomach modulating short-term appetitive control (i.e. to eat when the stomach is empty and to stop when the stomach is stretched). Leptin is produced by adipose tissue to signal fat storage reserves in the body, and mediates long-term appetitive controls (i.e. to eat more when fat storages are low and less when fat storages are high). Although administration of leptin may be effective in a small subset of obese individuals who are leptin deficient, most obese individuals are thought to be leptin resistant and have been found to have high levels of leptin. This resistance is thought to explain in part why administration of leptin has not been shown to be effective in suppressing appetite in most obese people.
A graphic depiction of a leptin molecule
While leptin and ghrelin are produced peripherally, they control appetite through their actions on the central nervous system. In particular, they and other appetite-related hormones act on the hypothalamus, a region of the brain central to the regulation of food intake and energy expenditure. There are several circuits within the hypothalamus that contribute to its role in integrating appetite, the melanocortin pathway being the most well understood. The circuit begins with an area of the hypothalamus, the arcuate nucleus, that has outputs to the lateral hypothalamus (LH) and ventromedial hypothalamus (VMH), the brain's feeding and satiety centers, respectively.
The arcuate nucleus contains two distinct groups of neurons. The first group coexpresses neuropeptide Y (NPY) and agouti-related peptide (AgRP) and has stimulatory inputs to the LH and inhibitory inputs to the VMH. The second group coexpresses pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART) and has stimulatory inputs to the VMH and inhibitory inputs to the LH. Consequently, NPY/AgRP neurons stimulate feeding and inhibit satiety, while POMC/CART neurons stimulate satiety and inhibit feeding. Both groups of arcuate nucleus neurons are regulated in part by leptin. Leptin inhibits the NPY/AgRP group while stimulating the POMC/CART group. Thus a deficiency in leptin signaling, either via leptin deficiency or leptin resistance, leads to overfeeding and may account for some genetic and acquired forms of obesity.
Management
The main treatment for obesity consists of dieting and physical exercise. Diet programs may produce weight loss over the short term, but keeping this weight off can be a problem and often requires making exercise and a lower calorie diet a permanent part of a person's lifestyle.Success rates of long-term weight loss maintenance are low and range from 2–20%. In a more structured setting, however, 67% of people who lost greater than 10% of their body mass maintained or continued to lose weight one year later. An average maintained weight loss of more than 3 kg (6.6 lb) or 3% of total body mass could be sustained for five years.
Some studies have found significant benefits in mortality in certain populations with weight loss. In a prospective study of obese women with weight related diseases, intentional weight loss of any amount was associated with a 20% reduction in mortality. In obese women without obesity related illnesses a weight loss of greater than 9 kg (20 lb) was associated with a 25% reduction in mortality. A recent review concluded that certain subgroups such as those with type 2 diabetes and women show long term benefits in all cause mortality, while outcomes for men do not seem to be improved with weight loss.A subsequent study has found benefits in mortality from intentional weight loss in those who have severe obesity.
The most effective treatment for obesity is bariatric surgery; however, due to its cost and the risk of complications, researchers are searching for other effective yet less invasive treatments.
Dieting
Diets to promote weight loss are generally divided into four categories: low-fat, low-carbohydrate, low-calorie, and very low calorie. A meta-analysis of six randomized controlled trials found no difference between three of the main diet types (low calorie, low carbohydrate, and low fat), with a 2–4 kilogram (4.4–8.8 lb) weight loss in all studies. At two years these three methods resulted in similar weight loss irrespective of the macronutrients emphasized.
Very low calorie diets provide 200–800 kcal/day, maintaining protein intake but limiting calories from both fat and carbohydrates. They subject the body to starvation and produce an average weekly weight loss of 1.5–2.5 kilograms (3.3–5.5 lb). These diets are not recommended for general use as they are associated with adverse side effects such as loss of lean muscle mass, increased risks of gout, and electrolyte imbalances. People attempting these diets must be monitored closely by a physician to prevent complications.
Exercise
Physical exercise
With use, muscles consume energy derived from both fat and glycogen. Due to the large size of leg muscles, walking, running, and cycling are the most effective means of exercise to reduce body fat. Exercise affects macronutrient balance. During moderate exercise, equivalent to a brisk walk, there is a shift to greater use of fat as a fuel. To maintain health the American Heart Association recommends a minimum of 30 minutes of moderate exercise at least 5 days a week.
A meta-analysis of 43 randomized controlled trials by the Cochrane Collaboration found that exercising alone led to limited weight loss. In combination with diet, however, it resulted in a 1 kilogram weight loss over dieting alone. A 1.5 kilogram (3.3 lb) loss was observed with a greater degree of exercise. Even though exercise as carried out in the general population has only modest effects, a dose response curve is found, and very intense exercise can lead to substantial weight loss. During 20 weeks of basic military training with no dietary restriction, obese military recruits lost 12.5 kg (27.6 lb). High levels of physical activity seem to be necessary to maintain weight loss. A pedometer appears useful for motivation. Over an average of 18-weeks of use physical activity increased by 27% resulting in a 0.38 decreased in BMI.
Signs that encourage the use of stairs as well as community campaigns have been shown to be effective in increasing exercise in a population. The city of Bogota, Colombia for example blocks off 113 kilometers (70 miles) of roads every Sunday and on holidays to make it easier for its citizens to get exercise. These pedestrian zones are part of an effort to combat chronic diseases, including obesity.
Weight loss programs
Weight loss programs often promote lifestyle changes and diet modification. This may involve eating smaller meals, cutting down on certain types of food, and making a conscious effort to exercise more. These programs also enable people to connect with a group of others who are attempting to lose weight, in the hopes that participants will form mutually motivating and encouraging relationships.
A number of popular programs exist, including Weight Watchers, Overeaters Anonymous, and Jenny Craig. These appear to provide modest weight loss (2.9 kg, 6.4 lb) over dieting on one's own (0.2 kg, 0.4 lb) over a two year period. Internet-based programs appear to be ineffective. The Chinese government has introduced a number of "fat farms" where obese children go for reinforced exercise, and has passed a law which requires students to exercise or play sports for an hour a day at school (see Obesity in China).
Medication
Anti-obesity medication
Orlistat (Xenical) the most commonly used medication to treat obesity and sibutramine (Meridia) a recently withdrawn medication due to cardiovascular side effects
Only one anti-obesity medications orlistat (Xenical) is currently approved by the FDA for long term use. It reduces intestinal fat absorption by inhibiting pancreatic lipase. Rimonabant (Acomplia), a second drug, works via a specific blockade of the endocannabinoid system. It has been developed from the knowledge that cannabis smokers often experience hunger, which is often referred to as "the munchies". It had been approved in Europe for the treatment of obesity but has not received approval in the United States or Canada due to safety concerns. European Medicines Agency in October 2008 recommended the suspension of the sale of rimonabant as the risk seem to be greater than the benefits. Sibutramine (Meridia), which acts in the brain to inhibit deactivation of the neurotransmitters, thereby decreasing appetite was withdrawn from the UK market in January of 2010 and United States and Canadian markets in October of 2010 due to cardiovascular concerns.
Weight loss with these drugs is modest. Over the longer term, average weight loss on orlistat is 2.9 kg (6.4 lb), sibutramine is 4.2 kg (9.3 lb) and rimonabant is 4.7 kg (10.4 lb). Orlistat and rimonabant lead to a reduced incidence of diabetes, and all three drugs have some effect on cholesterol. However, there is little information on how these drugs affect the longer-term complications or outcomes of obesity. In 2010 the FDA noted concerns that sibutramine increases the risk of heart attacks and strokes in people with a history of cardiovascular disease.
There are a number of less commonly used medications. Some are only approved for short term use, others are used off-label, and still others are used illegally. Most are appetite suppressants that act on one or more neurotransmitters.Phendimetrazine (Bontril), diethylpropion (Tenuate), and phentermine (Adipex-P) are approved by the FDA for short term use, while bupropion (Wellbutrin), topiramate (Topamax), and zonisamide (Zonegran) are sometimes used off-label. Recombinant human leptin is very effective in those with obesity due to congenital complete leptin deficiency via decreasing energy intake and possibly increases energy expenditure. This condition is, however, rare and this treatment is not effective for inducing weight loss in the majority of people with obesity. It is being investigated to determine whether or not it helps with weight loss maintenance.
The usefulness of certain drugs depends upon the comorbidities present. Metformin (Glucophage) is preferred in overweight diabetics, as it may lead to mild weight loss in comparison to sulfonylureas or insulin. The thiazolidinediones, on the other hand, may cause weight gain, but decrease central obesity. Diabetics also achieve modest weight loss with fluoxetine (Prozac), orlistat and sibutramine over 12–57 weeks. Preliminary evidence has however found higher number of cardiovascular events in people taking sibutramine verses control (11.4% vs. 10.0%). The long-term health benefits of these treatments remain unclear.
Fenfluramine and dexfenfluramine were withdrawn from the market in 1997,while ephedrine (found in the traditional Chinese herbal medicine má huáng made from the Ephedra sinica) was removed from the market in 2004. Dexamphetamines are not approved by the FDA for the treatment of obesity due to concerns regarding addiction and abuse potential. The use of these drugs is not recommended due to potential side effects. However, people do occasionally use these drugs illegally.
Surgery
Bariatric surgery
Bariatric surgery ("weight loss surgery") is the use of surgical intervention in the treatment of obesity. As every operation may have complications, surgery is only recommended for severely obese people (BMI > 40) who have failed to lose weight following dietary modification and pharmacological treatment. Weight loss surgery relies on various principles: the two most common approaches are reducing the volume of the stomach (e.g. by adjustable gastric banding and vertical banded gastroplasty), which produces an earlier sense of satiation, and reducing the length of bowel that comes into contact with food (gastric bypass surgery), which directly reduces absorption. Band surgery is reversible, while bowel shortening operations are not. Some procedures can be performed laparoscopically. Complications from weight loss surgery are frequent.
Surgery for severe obesity is associated with long-term weight loss and decreased overall mortality. One study found a weight loss of between 14% and 25% (depending on the type of procedure performed) at 10 years, and a 29% reduction in all cause mortality when compared to standard weight loss measures. A marked decrease in the risk of diabetes mellitus, cardiovascular disease and cancer has also been found after bariatric surgery. Marked weight loss occurs during the first few months after surgery, and the loss is sustained in the long term. In one study there was an unexplained increase in deaths from accidents and suicide, but this did not outweigh the benefit in terms of disease prevention. When the two main techniques are compared, gastric bypass procedures are found to lead to 30% more weight loss than banding procedures one year after surgery.
The effects of liposuction on obesity are less well determined. Some small studies show benefits while others show none. A treatment involving the placement of an intragastric balloon via gastroscopy has shown promise. One type of balloon led to a weight loss of 5.7 BMI units over 6 months or 14.7 kg (32.4 lb). Regaining lost weight is common after removal, however, and 4.2% of people were intolerant of the device.
Clinical protocols
Much of the Western world has created clinical practice guidelines in an attempt to address rising rates of obesity. Australia, Canada, the European Union, and the United States have all published statements since 2004.
In a clinical practice guideline by the American College of Physicians, the following five recommendations are made:
People with a BMI of over 30 should be counseled on diet, exercise and other relevant behavioral interventions, and set a realistic goal for weight loss.
If these goals are not achieved, pharmacotherapy can be offered. The person needs to be informed of the possibility of side-effects and the unavailability of long-term safety and efficacy data.
Drug therapy may consist of sibutramine, orlistat, phentermine, diethylpropion, fluoxetine, and bupropion. For more severe cases of obesity, stronger drugs such as amphetamine and methamphetamine may be used on a selective basis. Evidence is not sufficient to recommend sertraline, topiramate, or zonisamide.
In people with a BMI over 40 who fail to achieve their weight loss goals (with or without medication) and who develop obesity-related complications, referral for bariatric surgery may be indicated. The person needs to be aware of the potential complications.
Those requiring bariatric surgery should be referred to high-volume referral centers, as the evidence suggests that surgeons who frequently perform these procedures have fewer complications.
A clinical practice guideline by the US Preventive Services Task Force (USPSTF) concluded that the evidence is insufficient to recommend for or against routine behavioral counseling to promote a healthy diet in unselected people in primary care settings, but that intensive behavioral dietary counseling is recommended in those with hyperlipidemia and other known risk factors for cardiovascular and diet-related chronic disease. Intensive counseling can be delivered by primary care clinicians or by referral to other specialists, such as nutritionists or dietitians.
Canada developed and published evidence-based practice guidelines in 2006. The guidelines attempt to address the prevention and management of obesity at both the individual and population levels in both children and adults. The European Union published clinical practice guidelines in 2008 in an effort to address the rising rates of obesity in Europe. Australia came out with practice guidelines in 2004.
Epidemiology
Epidemiology of obesity
World obesity prevalence among males (left) and females (right).
<5% 5–10% 10–15% 15–20% 20–25% 25–30% 30–35% 35–40% 40–45% 45–50% 50–55% >55%
Before the 20th century, obesity was rare; in 1997 the WHO formally recognized obesity as a global epidemic. As of 2005 the WHO estimates that at least 400 million adults (9.8%) are obese, with higher rates among women than men. The rate of obesity also increases with age at least up to 50 or 60 years old and severe obesity in the United States, Australia, and Canada is increasing faster than the overall rate of obesity.
Once considered a problem only of high-income countries, obesity rates are rising worldwide and affecting both the developed and developing world. These increases have been felt most dramatically in urban settings. The only remaining region of the world where obesity is not common is sub-Saharan Africa.
Public health
The World Health Organization (WHO) predicts that overweight and obesity may soon replace more traditional public health concerns such as undernutrition and infectious diseases as the most significant cause of poor health. Obesity is a public health and policy problem because of its prevalence, costs, and health effects. Public health efforts seek to understand and correct the environmental factors responsible for the increasing prevalence of obesity in the population. Solutions look at changing the factors that cause excess calorie consumption and inhibit physical activity. Efforts include federally reimbursed meal programs in schools, limiting direct junk food marketing to children, and decreasing access to sugar-sweetened beverages in schools. When constructing urban environments, efforts have been made to increase access to parks and to develop pedestrian routes.
Many countries and groups have published reports pertaining to obesity. In 1998 the first US Federal guidelines were published, titled "Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report".In 2006 the Canadian Obesity Network published the "Canadian Clinical Practice Guidelines (CPG) on the Management and Prevention of Obesity in Adults and Children". This is a comprehensive evidence-based guideline to address the management and prevention of overweight and obesity in adults and children.
In 2004, the United Kingdom Royal College of Physicians, the Faculty of Public Health and the Royal College of Paediatrics and Child Health released the report "Storing up Problems", which highlighted the growing problem of obesity in the UK. The same year, the House of Commons Health Select Committee published its "most comprehensive inquiry [...] ever undertaken" into the impact of obesity on health and society in the UK and possible approaches to the problem. In 2006, the National Institute for Health and Clinical Excellence (NICE) issued a guideline on the diagnosis and management of obesity, as well as policy implications for non-healthcare organizations such as local councils.
A 2007 report produced by Sir Derek Wanless for the King's Fund warned that unless further action was taken, obesity had the capacity to cripple the National Health Service financially. In the United States organizations such as the Bill Clinton Foundation's Alliance for a Healthier Generation and Action for Healthy Kids are working to combat childhood obesity. Additionally, the Centers for Disease Control and Prevention co-hosted the first-ever Weight of the Nation Conference in 2009 with the goal of focusing national attention on the obesity epidemic.
Comprehensive approaches are being looked at to address the rising rates of obesity. The Obesity Policy Action (OPA) framework divides measure into 'upstream' policies, 'midstream' policies, 'downstream' policies. 'Upstream' policies look at changing society, 'midstream' policies try to alter individuals' behavior to prevent obesity, and 'downstream' policies try to treat currently afflicted people.
Economic impact
Services must accommodate obese people with specialist equipment such as much wider chairs.
In addition to its health impacts, obesity leads to many problems including disadvantages in employment and increased business costs. These effects are felt by all levels of society from individuals, to corporations, to governments.
The estimate range for annual expenditures on diet products is $40 billion to $100 billion in the US alone. In 1998, the medical costs attributable to obesity in the US were $78.5 billion or 9.1% of all medical expenditures, while the cost of obesity in Canada was estimated at CA$2 billion in 1997 (2.4% of total health costs).
Obesity prevention programs have been found to reduce the cost of treating obesity-related disease. However, the longer people live, the more medical costs they incur. Researchers therefore conclude that reducing obesity may improve the public's health, but it is unlikely to reduce overall health spending.
Obesity can lead to social stigmatization and disadvantages in employment. When compared to their normal weight counterparts, obese workers on average have higher rates of absenteeism from work and take more disability leave, thus increasing costs for employers and decreasing productivity. A study examining Duke University employees found that people with a BMI over 40 filed twice as many workers' compensation claims as those whose BMI was 18.5–24.9. They also had more than 12 times as many lost work days. The most common injuries in this group were due to falls and lifting, thus affecting the lower extremities, wrists or hands, and backs. The US state of Alabama Employees' Insurance Board approved a controversial plan to charge obese workers $25 per month if they do not take measures to reduce their weight and improve their health. These measures started in January 2010 and apply to those with a BMI of greater than 35 kg/m2 who fail to make improvements in their health after one year.
Some research shows that obese people are less likely to be hired for a job and are less likely to be promoted. Obese people are also paid less than their non-obese counterparts for an equivalent job. Obese women on average make 6% less and obese men make 3% less.
Specific industries, such as the airline and food industries, have special concerns. Due to rising rates of obesity, airlines face higher fuel costs and pressures to increase seating width. In 2000, the extra weight of obese passengers cost airlines US$275 million. Costs for restaurants are increased by litigation accusing them of causing obesity. In 2005 the US Congress discussed legislation to prevent civil law suits against the food industry in relation to obesity; however, it did not become law.
History and culture
Etymology
Obesity is from the Latin obesitas, which means "stout, fat, or plump." Ēsus is the past participle of edere (to eat), with ob (over) added to it. The Oxford English Dictionary documents its first usage in 1611 by Randle Cotgrave.
Historical trends
During the Middle Ages and the Renaissance obesity was often seen as a sign of wealth, and was relatively common among the elite: The Tuscan General Alessandro del Borro, attributed to Charles Mellin, 1645
The Greeks were the first to recognize obesity as a medical disorder. Hippocrates wrote that "Corpulence is not only a disease itself, but the harbinger of others". The Indian surgeon Sushruta (6th century BCE) related obesity to diabetes and heart disorders. He recommended physical work to help cure it and its side effects. For most of human history mankind struggled with food scarcity. Obesity has thus historically been viewed as a sign of wealth and prosperity. It was common among high officials in Europe in the Middle Ages and the Renaissance as well as in Ancient East Asian civilizations.
With the onset of the industrial revolution it was realized that the military and economic might of nations were dependent on both the body size and strength of their soldiers and workers. Increasing the average body mass index from what is now considered underweight to what is now the normal range played a significant role in the development of industrialized societies. Height and weight thus both increased through the 19th century in the developed world. During the 20th century, as populations reached their genetic potential for height, weight began increasing much more than height, resulting in obesity. In the 1950s increasing wealth in the developed world decreased child mortality, but as body weight increased heart and kidney disease became more common. During this time period insurance companies realized the connection between weight and life expectancy and increased premiums for the obese.
Many cultures throughout history have viewed obesity as the result of a character flaw. The obesus or fat character in Greek comedy was a glutton and figure of mockery. During Christian times food was viewed as a gateway to the sins of sloth and lust. In modern Western culture, excess weight is often regarded as unattractive, and obesity is commonly associated with various negative stereotypes. People of all ages can face social stigmatization, and may be targeted by bullies or shunned by their peers. Obesity is once again a reason for discrimination.
Venus of Willendorf created 24,000–22,000 BC
Public perceptions in Western society regarding healthy body weight differ from those regarding the weight that is considered ideal – and both have changed since the beginning of the 20th century. The weight that is viewed as an ideal has become lower since the 1920s. This is illustrated by the fact that the average height of Miss America pageant winners increased by 2% from 1922 to 1999, while their average weight decreased by 12%.On the other hand, people's views concerning healthy weight have changed in the opposite direction. In Britain the weight at which people considered themselves to be overweight was significantly higher in 2007 than in 1999. These changes are believed to be due to increasing rates of adiposity leading to increased acceptance of extra body fat as being normal.
Obesity is still seen as a sign of wealth and well-being in many parts of Africa. This has become particularly common since the HIV epidemic began.
The arts
The first sculptural representations of the human body 20,000–35,000 years ago depict obese females. Some attribute the Venus figurines to the tendency to emphasize fertility while others feel they represent "fatness" in the people of the time.Corpulence is, however, absent in both Greek and Roman art, probably in keeping with their ideals regarding moderation. This continued through much of Christian European history, with only those of low socioeconomic status being depicted as obese.
During the Renaissance some of the upper class began flaunting their large size, as can be seen in portraits of Henry the VIII and Alessandro del Borro. Rubens (1577–1640) regularly depicted full-bodied women in his pictures, from which derives the term Rubenesque. These women, however, still maintained the "hourglass" shape with its relationship to fertility. During the 19th century, views on obesity changed in the Western world. After centuries of obesity being synonymous with wealth and social status, slimness began to be seen as the desirable standard.
Size acceptance and the obesity controversy
Overweight people, such as U.S. President William Howard Taft, have been ridiculed at various times.
Fat acceptance movement
The principal goal of the fat acceptance movement is to decrease discrimination against people who are overweight and obese. However, some in the movement are also attempting to challenge the established relationship between obesity and negative health outcomes.
A number of organizations exist that promote the acceptance of obesity. They have increased in prominence in the latter half of the 20th century. The US-based National Association to Advance Fat Acceptance (NAAFA) was formed in 1969 and describes itself as a civil rights organization dedicated to ending size discrimination.
The International Size Acceptance Association (ISAA) is a non-governmental organization (NGO) which was founded in 1997. It has more of a global orientation and describes its mission as promoting size acceptance and helping to end weight-based discrimination. These groups often argue for the recognition of obesity as a disability under the US Americans With Disabilities Act (ADA). The American legal system, however, has decided that the potential public health costs exceed the benefits of extending this anti-discrimination law to cover obesity.
Multiple books such as The Diet Myth by Paul Campos argue that the health risks of obesity are mostly unproven and the real problem is the social stigma facing the obese. Similarly, The Obesity Epidemic by Michael Gard argues that obesity is a moral and ideological construct, rather than a health problem. Other groups are also trying to challenge obesity's connection to poor health. The Center for Consumer Freedom, an organization partly supported by the restaurant and food industry, has run ads saying that obesity is not an epidemic but "hype".
People are known to select potential partners based on a similar body mass. The rising rates of obesity have therefore provided greater opportunities for overweight people to find partners. Certain subcultures also label themselves as particularly attracted to the obese. Chubby culture] and fat admirers are examples.
Research
Lorcaserin has been found to be effective in the treatment of obesity with a weight loss of 5.8 kg at one year as opposed to 2.2 kg with placebo. It however, failed to get FDA approval in 2010 due to concerns regarding cancer. Temporary, controllable gastric pseudo-bezoars (swallowable, swellable foreign bodies in the stomach meant to reduce gastric volume from inside the organ) are being tested. Treatment with naltrexone plus bupropion in a phase three trial resulted in a weight lose of 5–6% versus 1% for a placebo. Another combination that is in trials is phentermine and topiramate (Qnexa). In October of 2010 the FDA refused approval due to inadequate evidence regarding potential birth defects and cardiac side effects.
Childhood obesity
Childhood obesity
The healthy BMI range varies with the age and sex of the child. Obesity in children and adolescents is defined as a BMI greater than the 95th percentile. The reference data that these percentiles are based on is from 1963 to 1994 and thus has not been affected by the recent increases in rates of obesity. Childhood obesity has reached epidemic proportions in 21st century, with rising rates in both the developed and developing world. Rates of obesity in Canadian boys have increased from 11% in 1980s to over 30% in 1990s, while during this same time period rates increased from 4 to 14% in Brazilian children.
As with obesity in adults, many different factors contribute to the rising rates of childhood obesity. Changing diet and decreasing physical activity are believed to be the two most important in causing the recent increase in the rates. Because childhood obesity often persists into adulthood and is associated with numerous chronic illnesses, children who are obese are often tested for hypertension, diabetes, hyperlipidemia, and fatty liver. Treatments used in children are primarily lifestyle interventions and behavioral techniques. Medications are not FDA approved for use in this age group.
In other animals
Obesity in pets
Obesity in pets is common in many countries. Rates of overweight and obesity in dogs in the United States range from 23% to 41% with about 5.1% obese. Rates of obesity in cats was slightly higher at 6.4%. In Australia the rate of obesity among dogs in a veterinary setting has been found to be 7.6%. The risk of obesity in dogs is related to whether or not their owners are obese; however, there is no similar correlation between cats and their owners.
(source:wikipedia)





No comments:
Post a Comment